Everything You Need to Know About Blood Types – Part 1
The precise amount of blood in a person’s body will depend on their size. In addition, the blood’s composition varies between individuals. This difference in structure is what makes a person’s blood type. An individual’s blood type depends on which genes they inherited from their parents.
ABO is the best-known system for grouping blood types, though there are other methods. There are four major categories within the ABO group: A, B, O, and AB. Within these groups, there are a further eight blood types.
What Makes a Blood Type?
Doctors often use the ABO grouping system to classify blood types.
The main components of blood are:
- red blood cells, which carry oxygen around the body
- white blood cells, which play a crucial role in the immune system
- plasma, which is a yellowish liquid that contains proteins and salts
- platelets, which enable clotting
The blood group will depend on which antigens are on the surface of the red blood cells. Antigens are molecules. They can be either proteins or sugars. The types and features of antigens can vary between individuals, due to small genetic differences.
The antigens in blood have various functions, including:
- transporting other molecules into and out of the cell
- maintaining the structure of red blood cells
- detecting unwanted cells that could cause illness
Scientists use two types of antigens to classify blood types, ABO antigens and Rh antigens. Antigens and antibodies play a role in the immune system’s defense mechanism. White blood cells produce antibodies. These antibodies will target an antigen if they consider it a foreign object. Therefore, it is essential to match blood types when a person needs a transfusion.
ABO and the Most Common Blood Types
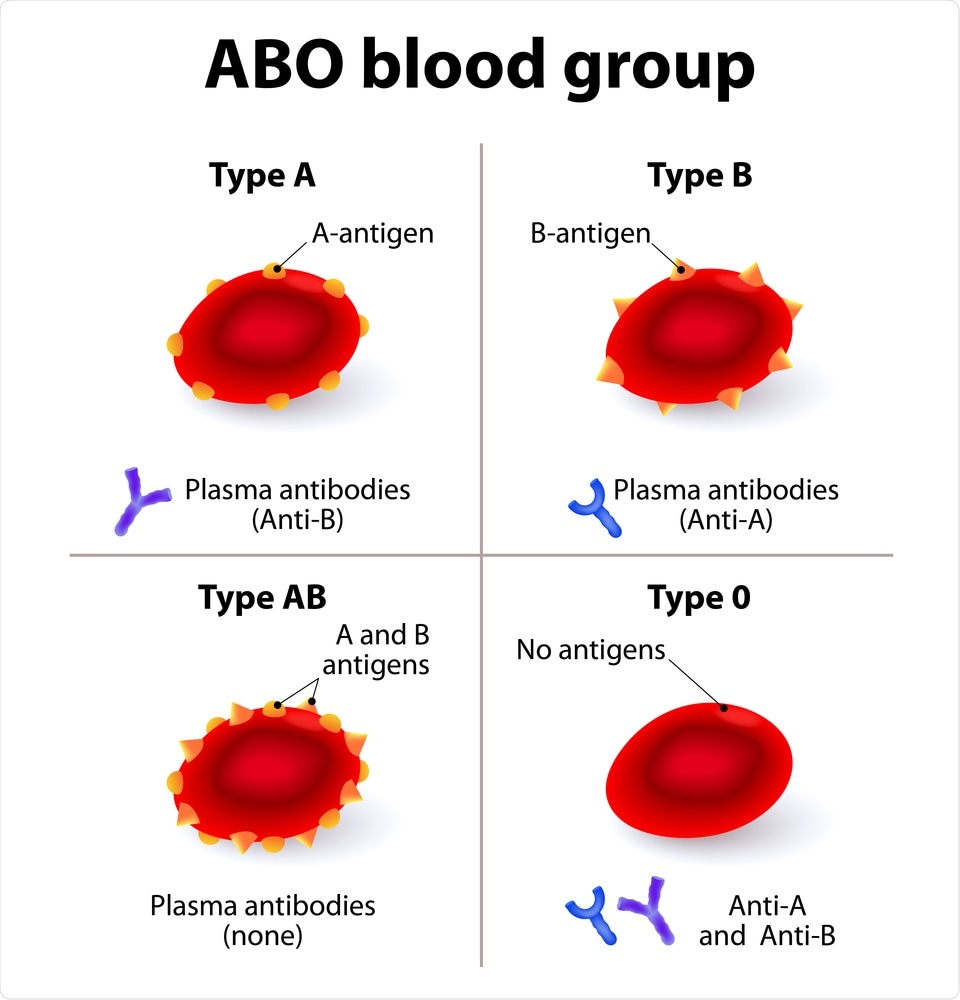
The ABO blood group system classifies blood types according to the different types of antigens in the red blood cells and antibodies in the plasma. They use the ABO system alongside the RhD antigen status to determine which blood type or types will match for a safe red blood cell transfusion.
There are four ABO groups:
Group A: The surface of the red blood cells contains A antigen, and the plasma has anti-B antibody. Anti-B antibody would attack blood cells that contain B antigen.
Group B: The surface of the red blood cells contains B antigen, and the plasma has anti-A antibody. Anti-A antibody would attack blood cells that contain A antigen.
Group AB: The red blood cells have both A and B antigens, but the plasma does not contain anti-A or anti-B antibodies. Individuals with type AB can receive any ABO blood type.
Group O: The plasma contains both anti-A and anti-B antibodies, but the surface of the red blood cells does not contain any A or B antigens. Since these antigens are not present, a person with any ABO blood type can receive this type of blood.
Rhesus Factor
Some red blood cells have Rh factor, also known as the RhD antigen. Rhesus grouping adds another dimension. If the red blood cells contain the RhD antigen, they are RhD positive. If they do not, they are RhD negative.
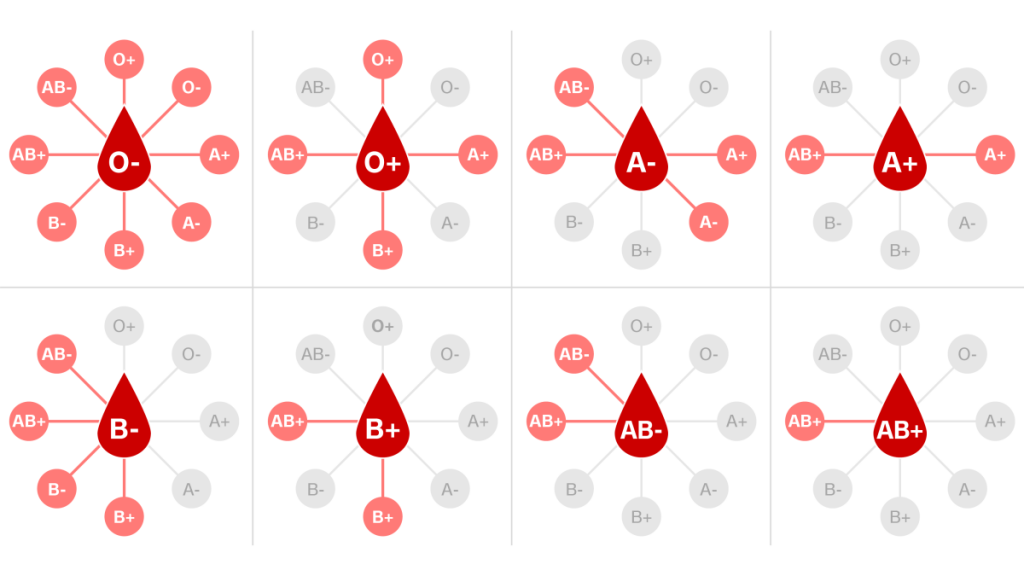
Doctors need to take into account both ABO and Rh when considering blood types. This means there are eight main blood types in the ABO/Rh blood group system. Some are more common than others.
These are the main types. Within the eight main groups, are there also many lesser-known and less common blood types.
Universal Donor and Universal Recipient
O negative blood contains no A, B, or RhD antigens. Almost anyone with any blood type can receive these red blood cells. A person with group O negative blood is a universal donor.
- A person with O-negative blood can donate to almost anyone.
- A person with Rh-negative blood can donate to a person with Rh-negative or Rh-positive blood.
- A person with Rh-positive blood can only donate to someone with Rh-positive blood.
As a result, there is a high demand for O negative blood, even though fewer than 10% of the U.S. population has this type. The rules for plasma are the opposite of those for Rh. A universal plasma donor will have type AB blood.
Risks and Compatibility
Before a person receives donated blood, doctors will check that this blood is compatible. Giving someone the wrong blood type can lead to potentially life-threatening reactions and complications.
If someone with group B antigen receives red blood cells from someone with group A antigen, their body will launch an immune response and reject the transfusion. The anti-A antibody in the recipient’s plasma will attack and destroy the A antigen donor red blood cells.
When the recipient’s plasma attacks and destroys the donor cells, the blood may clump, or agglutinate. This can lead to blood clots, which can obstruct blood vessels. If they break, hemoglobin can leak out, and this can be toxic.
Other possible adverse effects include allergic reactions and anaphylaxis. In some cases, the body can cope, but others can be life-threatening. Some reactions occur at once, while others can take up to 28 days to appear.
The subject of blood groups and their importance to people is too vast to cover in one article. Check back soon for future installments and more information.