Everything You Need to Know About Blood Types – Part 2
Welcome back to our series of articles on everything you need to know about blood types. In this article, we’ll be exploring blood type inheritance and how different rhesus groups can affect pregnancy.
How Does Blood Type Affect Pregnancy?
It’s important for women to find out their blood type at the start of their pregnancy. Blood will be taken to find this out. As previously mentioned, there are four different types: A, B, AB and O.
In addition to blood type, women can have Rh factor (specifically Rhesus D antigen), which is when proteins appear on the surface of the blood. Women who do have Rh factor are classified as Rh positive (A+, B+, AB+ and O+) and women who don’t are Rh negative (A-, B-, AB- and O).
The blood type and Rh factor of a pregnant woman and the father of her baby can affect what blood type the baby has. It will also influence the antibodies the mother’s body makes as an immune response to foreign matter in her body such as bacteria, sperm and even an embryo.
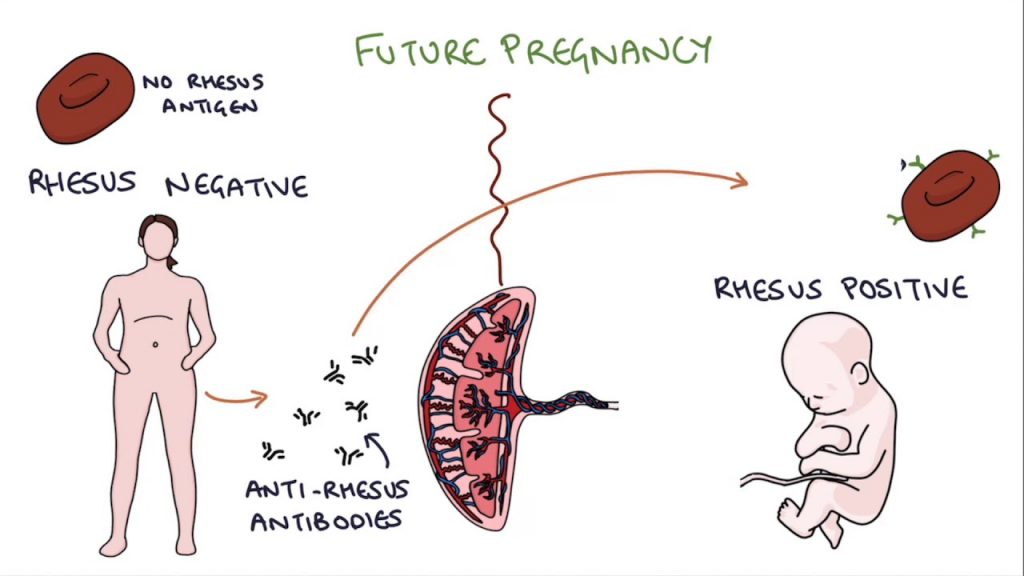
When an Rh-negative woman (5-10 percent of women) has a baby with Rh-positive blood this is called Rh incompatibility. The mother’s body will treat the Rh proteins found in her baby’s blood as foreign and make antibodies to attack them, as soon as the two blood types mix in any way, which is a condition called Rhesus disease.
There can also sometimes be problems if a mother is an O blood type and her baby is A or B blood type, where the mother’s body produces antibodies against the baby’s red blood cells when blood mixes. This is called ABO incompatibility.

What are the Risk Factors?
The first time a woman is pregnant, the baby is generally protected until birth because the mother’s blood cannot cross the placenta (although small amounts of baby’s blood can get into the mother’s circulation).
However, there may be some instances where the baby’s blood and mother’s blood mixes sooner than this, such as:
- miscarriage
- an injury that causes bleeding (such as a car accident)
- after an amniocentesis (where blood is taken from the umbilical cord for testing)
- after a CVS (where a sample of the placenta is taken for testing)
- an ectopic pregnancy.
In any of these situations, the antibodies will have developed as an immune response which can cause the baby to have anemia and severe jaundice.
With Rh incompatibility, this means whenever the woman is pregnant with an Rh positive baby in the future, antibodies will be produced in higher amounts. ABO incompatibility does not become more serious with each subsequent pregnancy. However, ABO incompatibility can affect a baby until all the antibodies pass out of the baby’s system after they are born.
What’s the Treatment?
Because a baby’s blood group is usually unknown during pregnancy, all women who are Rhesus negative receive anti-D injections during pregnancy to prevent an onset of Rhesus disease at 28 and 34 weeks. Cord blood is collected at birth to check the baby’s blood group, and if the baby is Rhesus positive, another injection is given. These injections are very effective at stopping Rh antibodies developing and making it possible for women to be pregnant again without Rh incompatibility complications. If the baby is Rhesus negative, injections are not required.
If a woman has already been diagnosed with Rhesus disease while pregnant, she will be carefully monitored to make sure the baby is healthy, through ultrasound. If necessary, a doctor can check the baby for any signs of anemia by specialist ultrasound monitoring and intervention.
If at any time the baby’s blood count is too low, special blood exchange transfusions (either before or after birth) can be given to the baby via the umbilical cord, to stop depletion of the red blood cells and occasionally a baby may need to be delivered early. However, these things aren’t usually necessary as anti-D injections are very successful.
With ABO incompatibility, there are no preventative measures to protect the baby but if a baby is showing any signs of anemia in-utero or is very jaundiced after being born, they will be given phototherapy to help break down the chemicals in their blood that are causing their jaundice, and may also need blood transfusions if they are very anemic. All this will be done straight after birth to prevent any long-term problems.
Does it Affect the Mother?
The mother’s health won’t be affected by blood type incompatibility, but bleeding of any kind while pregnant is something women should always speak to their doctor about, as it can indicate a problem besides Rh incompatibility or ABO incompatibility.
Has this article been helpful to you? Let us know in the comments below.




Blood incompatibility needs to be treated during pregnancy. Otherwise, it may cause serious problems.
https://babycare-all.com/how-to-deal-with-blood-incompatibility-in-pregnancy/